Pediatric Cancer Recurrence Prediction is an exciting development in the realm of pediatric oncology, particularly for children diagnosed with gliomas. Recent advancements in artificial intelligence have introduced robust tools that significantly enhance the accuracy of predicting cancer relapse in young patients. By utilizing MRI scans over time, these AI systems analyze subtle changes that could indicate an increased risk of recurrence, thereby improving brain cancer prognosis. This innovation not only alleviates the stress of frequent medical imaging but also allows for tailored treatment approaches in pediatric patients. As healthcare technology evolves, the integration of AI in pediatric cancer management shines a beacon of hope for families navigating the challenges of childhood cancer.
The prediction of recurrence in childhood cancers is gaining considerable attention, especially with the implementation of advanced AI technologies. These innovations allow clinicians to utilize a series of MRI scans from pediatric patients, offering a clearer picture of potential tumor regrowth in cases like glioma treatment. Improved diagnostic tools in pediatric oncology not only enhance the precision of relapse detection but also assist in creating a more personalized care plan for young cancer survivors. Throughout this evolution in medical imaging, the quest for increased MRI scan accuracy in cancer continues to play a vital role in shaping future treatment protocols. By fostering a multidisciplinary approach, healthcare providers aim to support families better while promoting long-term well-being amid the uncertainties of brain cancer.
The Role of AI in Pediatric Oncology
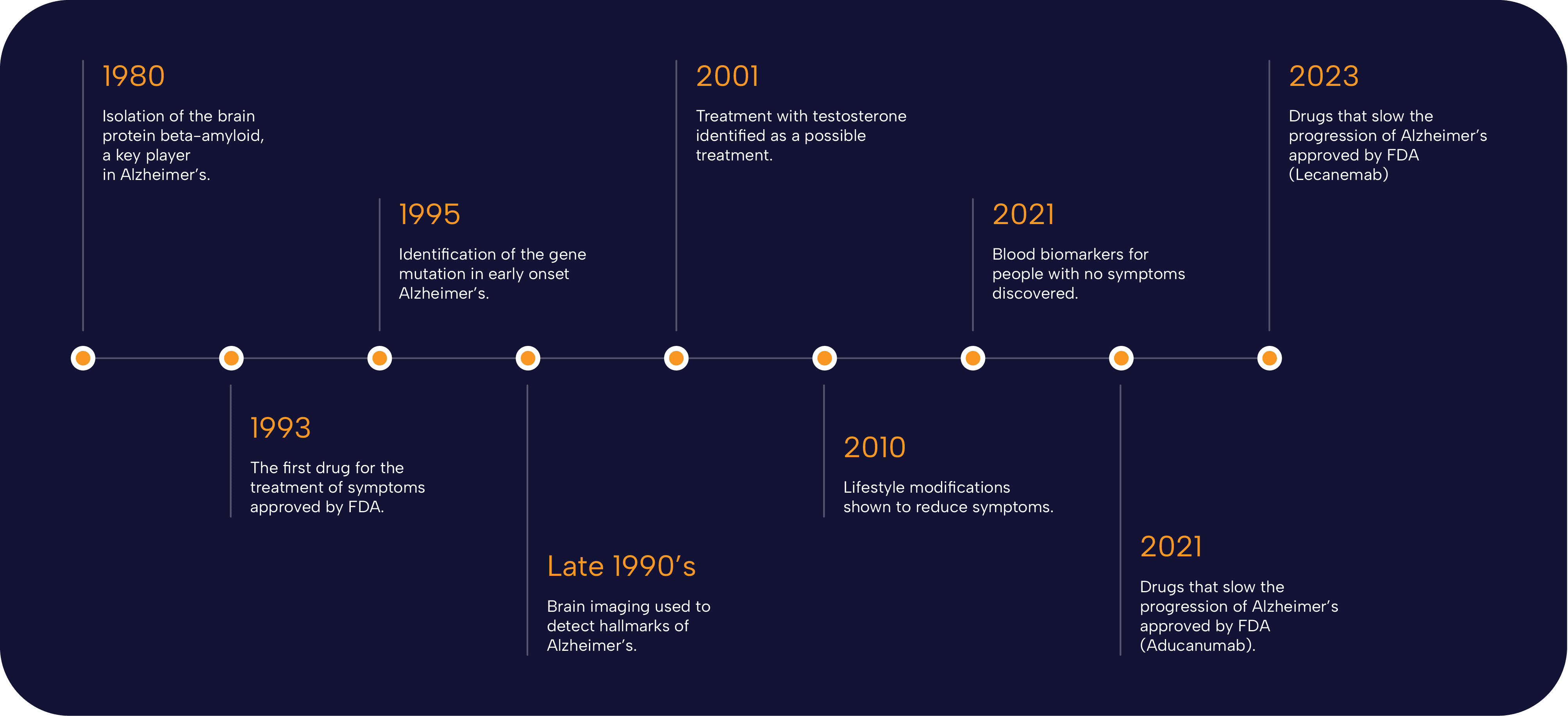
Artificial Intelligence (AI) is reshaping the landscape of pediatric oncology by introducing advanced tools that enhance diagnosis and treatment strategies. AI algorithms analyze extensive data sets to identify patterns and trends in childhood cancer cases, leading to more accurate prognoses. By collecting data from various sources such as MRI scans and historical patient outcomes, AI can assist healthcare providers in making informed decisions about treatment plans. This proactive approach not only improves the efficacy of therapies but also alleviates some of the anxiety that families experience during treatment.
Moreover, the integration of AI tools into pediatric oncology has led to a decline in the time taken to analyze imaging results. Traditional methods rely heavily on the experience and intuition of radiologists, which can vary significantly. In contrast, AI tools deliver consistent and objective assessments, particularly when dealing with complex cases like gliomas. For instance, predictive analyses help clinicians understand which patients may face complications or cancer recurrence, thus enabling tailored follow-up strategies and improving overall health outcomes.
Pediatric Cancer Recurrence Prediction Using AI
The prediction of pediatric cancer recurrence has traditionally been fraught with uncertainties, primarily due to the complexities involved in different tumor behaviors among children. Today, thanks to innovative AI tools, oncologists can make more accurate predictions regarding relapse risks. Recent studies indicate that AI models can predict the likelihood of glioma recurrence with significantly higher accuracy compared to conventional methods. This development is crucial, as timely intervention can vastly improve the prognosis and quality of life for young patients.
Backed by studies like those from Mass General Brigham, researchers are harnessing advanced AI techniques, such as temporal learning, to analyze multiple MRI scans over time. This method allows the AI to identify subtle changes in tumor behavior that single scans might miss, creating a more comprehensive risk assessment. The findings suggest that AI can help determine which patients are at the highest risk of recurrence, enabling oncologists to implement more personalized treatment pathways, reduce stress on families through fewer unneeded scans, and ultimately enhance overall pediatric cancer care.
Enhancing Brain Cancer Prognosis Through AI Tools
The prognosis for brain cancer in pediatric patients is rapidly evolving, with AI playing a pivotal role in improving outcomes. Advanced algorithms have the capability to process large datasets from various imaging techniques, providing insights that ought to guide treatment decisions. For example, AI not only assists in diagnosing conditions like gliomas but also offers predictive capabilities for treatment outcomes, enabling tailored management that meets the specific needs of each child. It is increasingly evident that employing AI in clinical settings is revolutionizing how healthcare providers approach brain cancer in children.
By incorporating AI tools into the diagnostic framework for pediatric oncology, medical professionals can enhance their understanding of how certain tumors react differently in young patients. The integration of detailed MRI scan assessments with AI predictions allows for an informed dialogue between doctors and families about potential treatment routes, side effects, and the long-term prognosis of brain cancer patients. Given that each child’s body reacts uniquely to treatment, leveraging these intelligent tools marks a significant stride towards personalized oncology care.
The Impact of MRI Scan Accuracy in Cancer Treatment
MRI scans are integral to the detection and monitoring of brain tumors in pediatric patients. The accuracy garnered from AI-assisted MRI evaluations significantly improves the detection of tumor changes over time, providing case-specific insights that were previously unattainable. By utilizing advanced imaging analysis techniques, radiologists can identify tumor recurrences or shifts in growth patterns much earlier, allowing for prompt intervention. This attention to detail is especially crucial in the context of gliomas, where the treatment approach can pivot based on subtle changes that may indicate a resurgence of the disease.
Furthermore, enhanced MRI scan accuracy provides families with a clearer understanding of their child’s condition. Instead of waiting for potentially misleading single-scan results, families can receive informed assessments based on comprehensive data drawn from the AI’s analysis. This clarity can significantly reduce the emotional burden on families, fostering a more transparent relationship with healthcare providers. Emphasizing this accurate monitoring through AI technologies not only improves patient care but also instills confidence in both the families and the medical teams involved.
Innovations in Glioma Treatment and Monitoring
The advancement of treatment protocols for pediatric gliomas is witnessing unprecedented changes with the help of AI technologies. New approaches utilizing AI-driven imaging assessments allow for better tracking of tumor growth and response to therapies. These innovations facilitate more accurate evaluations of treatment efficacy, helping oncologists make well-informed decisions about ongoing and future interventions. By accurately monitoring the disease trajectory, healthcare providers can adapt treatment plans dynamically, offering hope for improved outcomes in pediatric brain cancer cases.
Moreover, as glioma treatment continues to evolve, the incorporation of AI into clinical practice offers the potential to uncover new therapeutic options. Investigations into targeted therapies, guided by AI analyses, can provide additional avenues for managing these challenging tumors. Ultimately, as more tools become available, the management and prognostic outcomes for children with gliomas stand to improve drastically, reinforcing the importance of integrating technology into contemporary medical practices.
Emphasizing Continuous Research for Pediatric Cancer Care
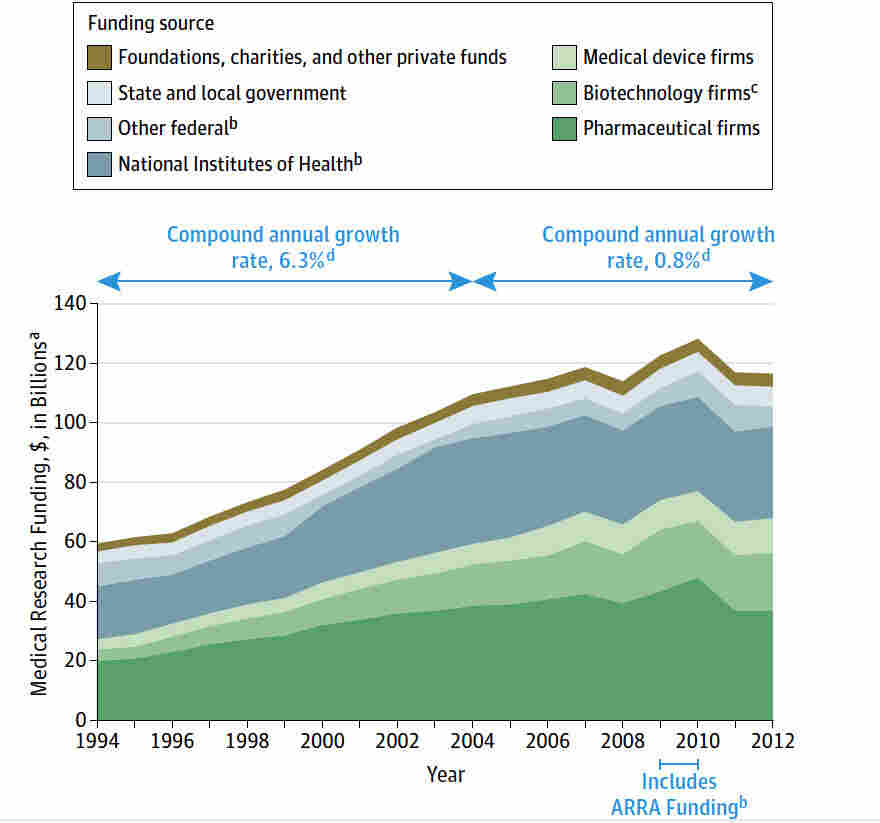
Continuous research is vital in the realm of pediatric cancer care, especially as new technologies like AI emerge. Ongoing studies are not only refining existing treatments but also exploring novel methodologies that could lead to breakthroughs in understanding tumor biology and recurrence predictions. As researchers engage with multidisciplinary teams, including AI experts, there is immense potential to develop more sophisticated tools that could elevate patient outcomes. By remaining committed to exploring these frontiers, the healthcare community can continually adapt to the changing landscape of pediatric oncology.
Another aspect of research focus is ensuring that the advancements in AI and imaging techniques are validated across diverse patient demographics. As new findings are published, the healthcare community must prioritize clinical trials to ascertain the effectiveness and utility of these technologies. By fostering an environment of rigorous scientific inquiry, the potential for translating AI advancements into mainstream pediatric cancer protocols will not only enhance treatment efficacy but also contribute to a more comprehensive understanding of cancer care in children.
Collaboration in Pediatric Cancer Research
Collaboration among research institutions and healthcare facilities plays an instrumental role in advancing pediatric cancer care. Groundbreaking studies require a concerted effort from various specialists, including oncologists, radiologists, and AI researchers. The synergy from such multidisciplinary collaborations can lead to innovations that encapsulate multiple dimensions of patient care—from diagnosis and treatment to surveillance of disease progression. Notably, the combined efforts of institutions like Mass General Brigham and Boston Children’s Hospital are cultivating an environment that fosters significant progress in the field.
Furthermore, sharing resources, including vast data sets from imaging and treatment outcomes, enables researchers to enhance the AI models currently in development. This pooling of knowledge contributes to more robust predictive analytics, enhancing understanding of cancer recurrence and treatment pathways. The cultivation of collaborative networks is essential not only for scientific discovery but also for ensuring that advancements in pediatric oncology translate effectively into practice, ultimately benefiting the patients and families involved.
Future Perspectives on AI in Pediatric Oncology
The future of AI in pediatric oncology appears promising, with advancements that could redefine diagnostic and treatment paradigms. As researchers continue to refine AI algorithms, the capacity to analyze complex physiological data in real-time will enhance the decision-making process for clinicians. This could lead to a revolution in predictive analytics, allowing for personalized care that tailors interventions based on individual tumor behaviors and responses to therapy. Excitingly, the objective is to reduce uncertainty around cancer treatment, allowing for safer and more effective management of pediatric cancer cases.
Emphasis on developing AI tools that are easy to integrate into existing medical frameworks is also key. Designing user-friendly interfaces and workflows will ensure that healthcare providers can engage with the technology effectively without a steep learning curve. As the synergy between AI and pediatric oncology grows stronger, it is anticipated that patient outcomes will significantly improve, paving the way for a new era in childhood cancer treatment where recurrence can be predicted and managed with unprecedented accuracy.
Frequently Asked Questions
How does AI in pediatric oncology improve pediatric cancer recurrence prediction?
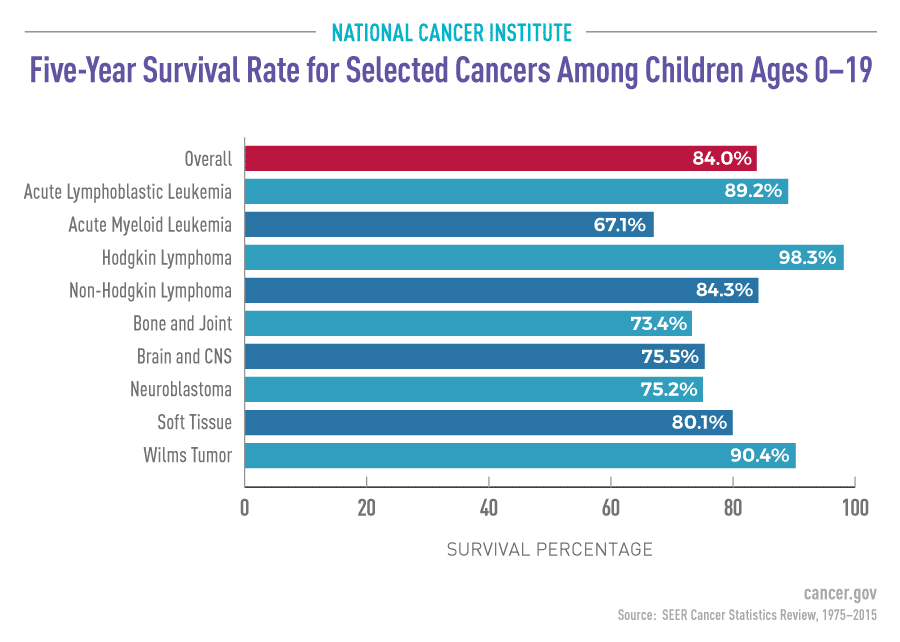
AI in pediatric oncology enhances pediatric cancer recurrence prediction by analyzing multiple MRI scans over time. This advanced approach, known as temporal learning, significantly increases accuracy—up to 75-89%—compared to traditional methods, which only achieve about 50%. By effectively interpreting subtle changes in brain scans, AI tools provide earlier warnings of potential relapses in pediatric cancer patients, particularly those with gliomas.
What is the significance of MRI scan accuracy in cancer recurrence prediction for pediatric patients?
MRI scan accuracy plays a crucial role in pediatric cancer recurrence prediction by allowing healthcare providers to identify subtle changes in brain tumors over time. Utilizing advanced AI models, such as those incorporating temporal learning, improves the predictive power related to relapse risks in children, offering more tailored follow-up care and treatment plans for pediatric cancer patients.
How are pediatric cancer AI tools utilized in predicting glioma treatment outcomes?
Pediatric cancer AI tools leverage advanced algorithms to analyze historical MRI data and imaging patterns, enhancing the prediction of recurrence in glioma treatment outcomes. By employing temporal learning, these AI systems can detect disease progression with greater precision, helping clinicians to better assess which pediatric patients are at higher risk for relapse and adjust their treatment protocols accordingly.
What impact does accurate brain cancer prognosis have on pediatric cancer care?
Accurate brain cancer prognosis, facilitated by AI in pediatric oncology, significantly improves patient care by enabling more personalized treatment plans. With precise predictions of pediatric cancer recurrence, healthcare providers can either minimize unnecessary imaging for low-risk patients or intervene proactively with targeted therapies for those identified at high risk, ultimately enhancing outcomes and reducing stress for patients and families.
Can AI predict pediatric cancer recurrence effectively for all types of brain tumors?
While AI shows promising capabilities in predicting pediatric cancer recurrence for gliomas, its effectiveness may vary with different types of brain tumors. Current studies indicate higher accuracy rates for low- and high-grade gliomas. However, continued research and validation in diverse clinical settings are essential to determine the generalizability of AI predictive models across various pediatric brain cancers.
What future developments are anticipated for pediatric cancer recurrence prediction using AI?
Future developments in pediatric cancer recurrence prediction using AI are likely to include more extensive clinical trials that validate current findings and further refine predictive algorithms. Researchers aim to explore broader applications of temporal learning across different tumor types and improve risk stratification processes, ultimately leading to enhanced clinical decision-making and patient outcomes in pediatric oncology.
| Key Points | Details |
|---|---|
| AI Tool Effectiveness | An AI tool predicts pediatric cancer relapse with 75-89% accuracy, outperforming single scan methods. |
| Temporal Learning | Utilizes multiple brain scans over time to improve prediction accuracy. |
| Study Collaboration | Conducted by Mass General Brigham, Boston Children’s Hospital, and others with 4,000 MRI scans from 715 patients. |
| Clinical Implications | Aimed at reducing frequent MRI follow-ups and enhancing personalized patient care. |
| Current Limitations | Further validation required before clinical use and potential for clinical trials. |
Summary
Pediatric Cancer Recurrence Prediction is being revolutionized by advanced AI tools, capable of making highly accurate predictions on relapse risks in young patients. This innovative approach, utilizing temporal learning with sequential MRI scans, marks a significant advancement over traditional methods, providing hope for personalized treatment strategies and optimized patient care.